Surgery: A vital cornerstone, mending lives and advancing healthcare progress.
Solving Healthcare Workflow Challenges with Technology
January 22, 2024
The recent announcement by the Ontario Government to expand the role of private surgical centers has ignited discussions about the potential impact on healthcare and Ontario Hospitals. However, the real elephant in the room may not be the introduction of private facilities but rather the underutilization and productivity challenges faced by existing surgical centers.
As someone deeply involved in healthcare innovation and transformation, I recognize the need for both within-the-box and out-of-the-box solutions to alleviate the strain on hospital surgical centers.
While considering innovative approaches, it’s essential to address the current underutilization issue within these centers, operating at a mere 70% utilization rate.
This raises critical questions about efficiency, resource optimization, and the overall sustainability of our healthcare system.
Private Surgical Clinics: The Productivity Wild Card
Private outpatient surgical centers are being explored as a potential solution to the productivity challenges faced by existing surgical centers. These specialized clinics, designed for high-volume procedures such as cataracts, joint replacements, and endoscopies, have demonstrated impressive efficiency gains. However, their deployment comes with unintended consequences, particularly in a geographically dispersed system like Canada’s, potentially exacerbating service inequality between urban and remote communities.
While private clinics offer benefits such as workflow optimization and elimination of variability, their proliferation may lead to increased complexity for existing surgical centers. The shift of complex cases back to these centers, coupled with reduced funding and heightened staffing demands, paints a challenging picture for traditional hospitals.
Bridging the Productivity Gap: A Call to Action
The bright side is that hospitals are recognizing the need to improve productivity within existing surgical centers. The underutilization of staffed hours, costing $20/minute, is a clear economic incentive to improve productivity. To address this, Ontario hospitals can leverage existing ‘Pockets of Excellence’ and scale best practices to enhance surgical department efficiency. This approach allows for improvements in patient care, reduced wait times, boosted staff morale, and the establishment of a financially sustainable healthcare system. The main drivers of productivity improvements in surgical centres are:
- First-Case Delays: Unpredictable factors contributing to delays beyond the control of block holders, including patient-related issues, supply chain disruptions, inadequate preparations, or delays by other team members.
- Intraoperative Time Estimation: Current inaccuracies in estimating intraoperative time, set weeks in advance by surgeons, with an accuracy level as low as 7%, further exacerbating underutilization.
- Room Turnaround Time: Influence of staff availability and priorities on room turnaround time, often based on proximity rather than predefined targets, standards, or visible priorities.
- Elective Surgery Time Allocation: The decentralized model of parceling elective surgery time into blocks allocated to individual surgeons, hindering coordination and resource sharing among block holders and operating rooms.
- Gridlocks and Patient Flow Challenges: Examples of gridlocks emerging from multiple operating rooms funneling into one Post Anesthesia Care Unit (PACU), resulting in patient hold-ups and surgery cancellations due to emergency surgeries or a lack of available surgical beds.
Pockets of Excellence: A Glimpse into Possibilities
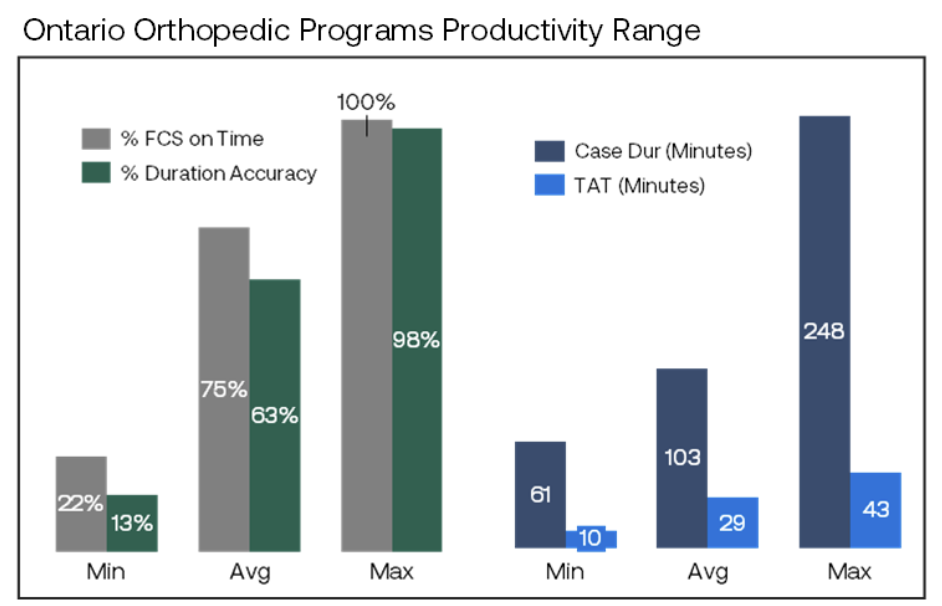
Reviewing 89 orthopedic surgical sites in Ontario that conduct 160,000 procedures yearly uncovers performance differences among providers. The range in some of the basic operating metrics (See Chart Below) shows the size of the opportunity when scaled across all providers and other surgeries. While no single hospital excels in all metrics, each demonstrates excellence in specific areas. Scaling these ‘Pockets of Excellence’ across programs and hospitals could potentially triple or quadruple the volume of surgeries within existing operating hours and staffing models – see Breaking Barriers: How One Hospital Redefined Surgical Efficiency.
A Comprehensive Approach to Future Success
To achieve these outcomes, a comprehensive approach is essential, encompassing technology adoption, process optimization, and collaborative strategies. Anticipating the current burning platform, many hospitals now have the opportunity to transform productivity and safeguard themselves, staff, and patients from the unintended consequences of more specialized surgical clinics.





